NON-SPECIFIC LOW BACK PAIN EXISTS. YOU JUST DON'T WANT TO ADMIT IT
Non specific low back pain is often a diagnosis that clinicians might feel sheepish about. As if they have failed. As if acknowledging uncertainty is a bad thing that leads to bad care. This isn’t true. It is quite often the only appropriate diagnosis and is the one that is the most accurate. Other acceptable diagnoses are non-specific shoulder pain. Or non-specific knee pain. Because when we say NSLBP we are acknowledging that NO ONE knows the specific anatomical source of nociception/pain. This is not really a debatable issue.
Before you freak out I would certainly note that it is still worth trying to find a specific diagnosis for our patients. Because sometimes they do exist and they are often sinister. But remember, a diagnosis has always been about the STRUCTURE. The structure that is CAUSING the pain. And if you are very honest with the literature we know that we can’t specifically target structures to elicit nociception and we certainly can’t say that a structure is causing pain. Pain is certainly much more multifactorial than that. And a non-specific structural diagnosis of pain opens us up to this wonderful complexity and can even improve our care.
If you think about it, even our “specific’ diagnoses aren’t really that specific. For example, what the hell does Patellofemoral Pain Syndrome actually mean? Your patient comes in and tells you it hurts around their knee cap when they squat and run. You have them squat, find that it hurts, maybe load the knee and find that it reproduces their knee ache, perhaps confirm that the pain isn’t referred from somewhere else and then boom. You put on your serious clinician face, pull out an anatomy text book and break the news that they have “Patellofemoral Pain Syndrome” Loosely translated as, “Knee cap on the leg bone pain syndrome”. Well, the patient just told you their knee cap hurt 30 minutes ago. You haven’t really arrived at some tissue specific diagnosis you’ve just paraphrased what they’ve said. You still don’t know the source of nociception and you certainly don’t know the source of pain.
The same thing holds with the majority of low back pain cases (Maher here). We don’t actually know the tissue source of pain. But this doesn’t mean that our treatment is non-specific. What does a good clinician then do with this anatomical uncertainty?
Working in just the biomechanical world the clinician finds the mechanical aggravators of the person. Some fancy tests like bending or twisting or jumping. When the patient says what movement hurts we then might relabel that simple description as “you have an Active-Extension Pattern”. This was a former classification seen in the CFT research group (but they no longer use this – Evolution is wonderful). But all it really says it what movements aggravates a patient’s pain. You can’t reliably infer what structure is sensitized and it doesn’t matter. That is not a diagnosis although many have advocated thru the years to call this a functional diagnosis. The same can be said if someone has pain flexing their spine. This might be called a flexion impairment or flexion intolerance. Again, this is not a diagnosis. You can’t infer what structure is sensitive from this. We are taught in school to consider the disc but the only research that tried to evaluate “pain” from a disc suggested that it was only the centralization of symptoms from the leg to the spine that would suggest a disc as the source of irritation (source here).
Calling a spine flexion intolerant is like diagnosing stomach pain but saying its burrito induced abdominal distress. That “diagnosis” is accurate and helpful (eat less burritos) but its not a true diagnosis – just like lbp diagnosis which merely catalogues aggravators.

But again, you don’t need that structural diagnosis anyway because it don’t change nuthin. If you are therapist who focuses on the mechanical aspects of irritation/pain then what do you do? For most therapists, treatment then gets tailored at addressing that sensitivity of that movement. Some of you will avoid the movement, some of you will poke into it, some of you will do something else that just desensitizes the person.
But lets change our lens a little bit here to point out why these functional diagnosis that are based on sensitive movements aren’t really diagnoses or how they don’t even see the full picture. If you think it’s a diagnosis to call low back pain “Extension induced low back pain” then what do you do if you treat with a broader mandate? Meaning you treat within the biopsychosocial model but focus on other areas that influence pain besides movement and mechanical loads.
You might be a therapist who focuses on the emotional and cognitive drivers of pain. We know that anxiety and depression are linked with pain. You might find with your validated tools that your patient has elevated levels of anxiety and depression and that these appear temporally linked with both the onset of pain and pain exacerbations. Do you then diagnosis the patient with Anxiety Intolerant Low Back Pain. You put in a treatment program that addresses these variables and the patient gets better. Aha, you had the right diagnosis. Or, not?
And what happens if you try to be a true biopsychosocialist. Looking for all the drivers, mediators, modulators, contributors, confounders, predisposers and (OK, you get the picture) of pain. You assess the same patient and find that a number of factors appear linked with pain. The patient:
- is sensitive to lumbar spine extension
- the onset was associated with repeated extension
- has elevated anxiety and has had bouts of depression
- has anxiety specifically related to pain and worry about damage
- has stopped engaging in meaningful activities
- believes their pain is due to the degenerative facet joint changes found on a x-ray (even though the changes were consistent with normal aging)
- actively engages in endurance coping behaviours where they continue to extend thinking that an upright posture is healthy
- has a spouse who tries to “help” by taking on their normal household duties
- they have a distorted body map of their low back
DOES RECOGNIZING THE MULTIDIMENSIONS OF PAIN ALLOW YOU TO BE MORE SPECIFIC?
All of the above factors may certainly be contributing to the patient’s pain. Do we now create a diagnosis word salad that incorporates all those contributors. E.g they have extension-anxiety-fear-rumination-cognitive-coping-normal homunculus intolerant low back pain?
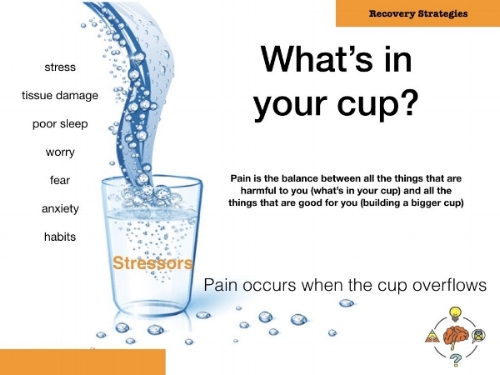
No, we don’t have to do that. We recognize that pain is complex. We still call this non-specific low back pain but now that we’ve done a thorough assessment we can see that there are a number of contributors. We have essentially figured out what is in their cup by listening to their story and doing a thorough exam.
We now try to either address what is in their cup of sensitivity or work with them to build a bigger cup.
When you recognize that pain is often structurally non specific it allows you to treat ALL of the factors that contribute to someone’s pain. Your treatment is much more tailored the individual than a treatment program predicated on some assumed structural or functional specificity.
If you want to learn more from Greg Lehman, check out his lecture on core stability here: Click here



